HYPERTENSION (High Blood Pressure)
The British Hypertension Society classification, defines mild hypertension as existing when the BP is above 140/90 mmHg.The Cardiovascular risks associated with high BP depend on the combination of risk factors in an individual, such as age, gender, weight, physical activity, smoking, family history, serum cholesterol, diabetes mellitus and pre-existing vascular disease.
Classification of Hypertension
Causes of Hypertension
Alcohol
Obesity
Pregnancy
RENAL DISEASE
- Glomerulonephritis
- Renal vascular disease
- Polycystic kidney disease
ENDOCRINE DISEASE
- Pheochromocytoma
- Cushing's syndrome
- Primary hyperaldosteronism (Conn's syndrome)
- Thyrotoxicosis
- Acromegaly
- Primary hypothyroidism
- Liddle's syndrome
- Congenital adrenal hyperplasia
COARCTATION OF THE AORTA
DRUGS
- Steroids : Anabolic steroids, corticosteroid, oral contraceptive pills.
- Cyclosporine
- Beta receptor agonists
- Sympathomimetics (Cold remedies/ Nasal drops)
- NSAIDs
Causes of isolated systemic hypertension
- Atherosclerosis
- Coarctation of aorta
- Severe AR
- Thyrotoxicosis
Pathogenesis
Hypertension has a number of adverse effects on the cardiovascular system.
In larger arteries (>1mm in diameter), the internal elastic lamina is thickened, smooth muscle is hypertrophied and fibrous tissue is deposited.
The vessels dilate and become tortuous, and their walls become less compliant.
In smaller arteries (<1mm), hyaline arteriosclerosis occurs in the wall, lumen narrows and aneurysms may develop.
Widespread atheroma developes and may lead to coronary and cerebrovascular disease.
These structural changes in the vasculature causes reduced renal blood flow, thereby activating the RENIN-ANGIOTENSIN-ALDOSTERONE AXIS.
Important environmental factors include:
- high salt intake
- heavy consumption of alcohol
- obesity
- lack of exercise
- Impaired intrauterine growth and low birth weight are associated with an increased risk of hypertension later in life.
How to measure blood pressure
Investigation
Investigation of Hypertension (All Patients)
- URINE ANALYSIS: Protein, glucose, haematuria
- Plasma Urea/ Creatinine
- Chest radiograph (Cardiomegaly, heart failure, rib notching)
- ECG (Left ventricular hypertrophy, ischaemia)
- Plasma electrolytes (hypokalaemia alkalosis in the absence of diuretic therapy may indicates primary or secondary hyperaldosteronism)
- Plasma cholesterol/ triglycerides.
Investigation of Hypertension (Patients Suspected of having Secondary Hypertension)
- Intravenous urogram, ultrasound (if renal disease is suspected)
- Radionuclide renography or renoarteriography (if there is evidence of renal artery stenosis)
- 24 hours urine catecholamines (VMA)
- Plasma renin activity and aldosterone (if Conn's disease is suspected)
- Urinary cortisol, dexamethasone suppression test (if signs of Cushing's syndrome is present)
- Angiography/MRI (if coarctation is suspected)
Management
Non-Drug therapy
Diet
- Weight reduction in obese and overweight patients (Aim: BMI < 25kg/m2)
- Avoid excess salt consumption (advised to restrict salt intake to 3 to 4 gm/day)
- Avoid alcohol
- Fat restriction
- Calcium, magnesium and potassium supplementation
- Fresh food preferred to processed food (as processed food has high salt content and decreased potassium content)
Exercise and Relaxation
- Regular exercise programme (isotonic exercise)
- Avoid isometric exercise
- Meditation
Smoking
Drug therapy
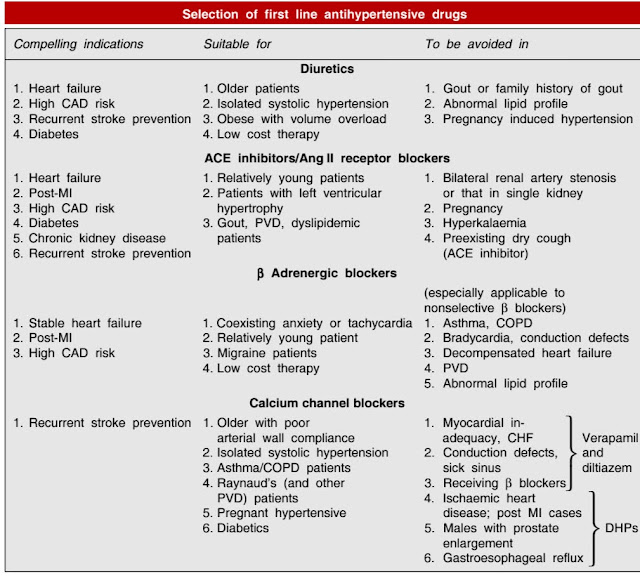
Diuretics
Thiazides: Hydrochlorothiazide, Chlorthalidone, Indapamide
High ceiling: Furosemide, etc.
Potassium sparing: Spironolactone, Amiloride
ACE inhibitors
Captopril, Enalapril, Lisinopril, Perindopril, Ramipril, Fosinopril, etc
Angiotensin (AT receptor) blockers
Losartan, Candesartan, Irbesartan, Valsartan, Telmisartan
Direct renin inhibitor
Aliskiren
Calcium channel blockers
Verapamil, Diltiazem, Nifedipine, Felodipine, Amlodipine, Nitrendipine, Lacidipine, etc.
Beta Adrenergic blockers
Propranolol, Metoprolol, Atenolol, etc.
Beta + alpha Adrenergic blockers
Labetalol, Carvedilol
Alpha Adrenergic blockers
Prazosin, Terazosin, Doxazosin, Phentolamine, Phenoxybenzamine
Central sympatholytics
Clonidine, Methyldopa
Vasodilators
Arteriolar: Hydralazine, Minoxidil, Diazoxide
Arteriolar + Venous: Sodium nitroprusside





Comments
Post a Comment
Please do not enter any spam link in the comment box.